As dental lab technicians, you play a crucial role in creating high-quality dental restorations that meet the expectations of both dentists and patients. When it comes to selecting the ideal material for a restoration, the choice between lithium disilicate and zirconia can be challenging. Both materials offer unique advantages and limitations, and understanding these differences is essential for achieving optimal results. In this blog post, we will compare lithium disilicate and zirconia restorations in terms of their properties, fabrication techniques, and clinical performance, to help dental lab technicians make informed decisions when choosing the best material for a specific case.
Lithium Disilicate:

- Strength: Lithium disilicate crowns offer good strength and high esthetics. They have a 10-year survival rate of 96.7%.
- Translucency: More translucent than zirconia, making it suitable for esthetic cases.
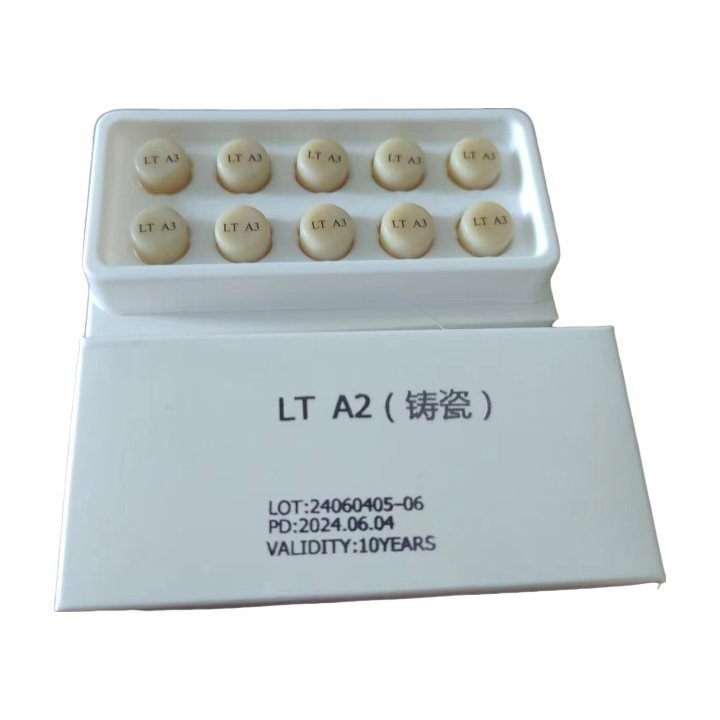
- Fabrication: Can be made using conventional (lost-wax hot-pressing) or CAD/CAM processes.
- Applications: Commonly used for anterior crowns and esthetic cases.
- Limitations: Posterior failures reported; abrasion of opposing enamel.
- Strength: Monolithic strength of 360 MPa.
Zirconia:
- Strength: Zirconia is often used for posterior restorations due to its biocompatibility, hardness, and fracture resistance.
- Translucency: Zirconia is less translucent than lithium disilicate but is more resistant.
- Fabrication: Zirconia is fabricated using CAD/CAM milling.
- Applications: Suitable for posterior crowns and bridges.
- Limitations: Aesthetics may not match natural teeth as closely as lithium disilicate.
Clinical Performance:
A systematic review found that both lithium disilicate and zirconia single crowns manufactured using CAD/CAM systems showed satisfactory clinical results. However, no definitive conclusions could be drawn due to limited studies and variations in methodologies.
Fabrication Techniques:
Lithium disilicate can be fabricated using hot-pressing or CAD/CAM methods. Hot-pressed lithium disilicate offers better internal fit and mechanical performance, which is advantageous for achieving optimal restoration outcomes.
Mechanical Properties:
Both lithium disilicate and zirconia-based materials have desirable mechanical properties such as high flexural strength and translucency. However, zirconia generally offers higher strength values, making it a preferred choice for more demanding clinical situations.
Aesthetics and Translucency:
Both materials can provide high aesthetic results. Lithium disilicate, especially in its advanced forms, can offer better translucency, which is crucial for achieving lifelike restorations.
Milling or Lost-Wax Casting:
Lithium disilicate can be milled from a block or produced through lost-wax casting. Milling allows for greater precision and control, while casting can offer a more natural appearance due to the material’s crystalline structure. Zirconia restorations are typically milled from a block, providing a consistent and precise restoration.
Conclusion:
Lithium disilicate and zirconia have unique advantages and limitations, making them suitable for different clinical situations. Lithium disilicate is generally preferred for anterior aesthetic cases due to its superior translucency and aesthetics. In contrast, zirconia is more commonly used for posterior restorations because of its high strength and wear resistance.
As dental lab technicians, it’s essential to consider the specific needs of each case and communicate closely with the dentist to determine the most appropriate material for the restoration. By understanding the unique properties and limitations of each material, dental lab technicians can make informed decisions and collaborate with dentists to provide the best possible restorations for their patients.


